By: Eriel Lauffer
Why We’re Talking About “Skin Infections” Today
Searches for the term skin infections top 8,100 a month, and a hefty chunk of those queries come from people living with—or suspecting they live with—Hidradenitis Suppurativa (HS). If that’s you, welcome. We’re HS Connect, a patient-powered hub that turns complex dermatology jargon into plain-English know-how. Today we’ll settle the great debate: skin infection vs HS. We’ll explain why HS abscesses look infected even when they’re not, how to spot a true infection, and how to treat a skin infection naturally while you wait for professional care.
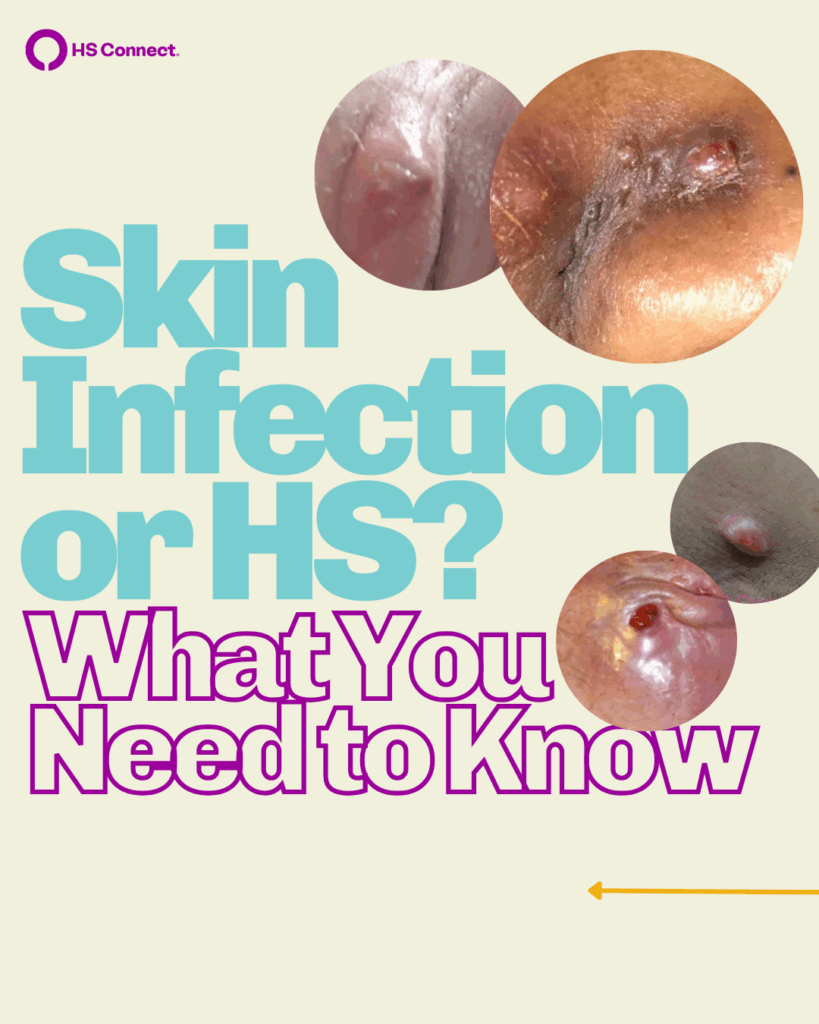
1. Infection or Inflammation? Debunking the Truth About HS Abscesses
HS is a chronic, inflammatory skin disease. Translation: your immune system is throwing a long-term party you didn’t invite. The result? Painful nodules and abscesses that are red, swollen, and tender—three adjectives most people associate with skin infections.
But here’s the kicker:
• Inflammation ≠ infection.
• HS abscesses can be completely sterile—zero bacteria—yet still look angry enough to scare your selfie camera.
1.1 The Science Bit (Super Condensed)
When your immune system targets the hair-follicle unit, the tunnel clogs, the area swells, and a pocket of pus forms. That pus is sterile until pathogenic bacteria break through the crowd. So redness alone is not proof of infection.
1.2 Why Does Every HS Flare Feel Infected?
- Heat + Blood Flow = Redness. Inflammation increases circulation, turning the skin ruby red.
- Pressure = Pain. Swelling stretches pain receptors.
- Leaking Fluid Looks Icky. Even sterile exudate resembles textbook infection drainage.
Put those together and you get the perfect mimic—an abscess that acts infected but isn’t.

2. Skin Infection vs HS: Your Quick-Glance Guide
| Feature | Classic Skin Infection | Hidradenitis Suppurativa Abscess |
|---|---|---|
| Root Cause | Pathogenic microbes, most often Staphylococcus aureus | Chronic immune-driven inflammation |
| Contagious? | Yes—can pass through skin-to-skin contact or shared items | No—HS is not contagious |
| Timeline | Acute; days to weeks | Chronic |
| Common Signs | Redness, warmth, pus, spreading edges, fever | Redness, tunnels, recurrent lumps, double-barrel drainage |
| Lab Culture | Positive for bacteria | Often negative or shows normal skin flora |
| First-Line Treatment | Antibiotics, incision & drainage (please see why I&Ds are NOT recommended for HS abscesses) | Anti-inflammatories, biologics, sometimes surgery |
| Natural Adjuncts | Warm compresses, antiseptic washes | Same, plus anti-inflammatory diet/lifestyle |
Bookmark that chart so you can wave it in front of every well-meaning neighbor who swears you “just need stronger antibiotics.”
3. The Role of Wound Cultures—And Why You Don’t Always Need One
Picture this: You visit urgent care, point to a flaming golf ball under your arm, and the clinician orders a swab. That culture serves three purposes:
- Confirm infection (or rule it out).
- Identify the perpetrator—MRSA, MSSA, or other.
- Match the bug to the drug—choosing an antibiotic that actually works.
For routine HS flares, cultures aren’t mandatory because most lesions aren’t infected. Cultures become crucial if you have:
• Fever or chills
• Rapidly spreading redness (think expanding bullseye)
• Unusual odor or color change
• Infection history with resistant organisms
4. Advanced Testing: When a Swab Isn’t Enough
Sometimes a standard culture comes back “no growth,” yet your skin insists otherwise. Enter 16S rRNA sequencing and full microbial genome panels. These sophisticated tests can map the entire bacterial neighborhood—including stealth organisms that refuse to grow in petri dishes. They’re pricey, often insurance-averse, and generally reserved for stubborn, non-healing wounds.
5. Risk Factors That Turn an HS Abscess Into a True Skin Infection
• Picking & Squeezing. Your fingernails are not surgical instruments.
• DIY Lancing. One dull sewing needle = open door for bacteria.
• Poor Hygiene Post-Drainage. Residual fluid feeds microbes.
• Occlusion & Humidity. Tight clothing traps sweat, creating a bacterial Jacuzzi.
• Impaired Immunity. Diabetes, steroid therapy, or biologics can lower defenses.
The most common complication is cellulitis—a skin-deep infection that spreads through surrounding tissue. Chronic offenders include repeat staph or MRSA colonization, which can bio-film themselves into Fort Knox.
6. How to Treat a Skin Infection Naturally (While Waiting for the Pros)
Natural remedies are adjuncts, not replacements, for medical treatment. If you suspect a true infection—fever, rapid spread, foul smell—call your healthcare provider ASAP. For mild cases or supportive care, consider these evidence-backed options:
6.1 Warm Compress Therapy
• Soak a clean washcloth in hot (not scalding) water.
• Apply 10–15 minutes, 3–4 times daily.
Benefits: increases circulation, encourages spontaneous drainage, soothes pain.
6.2 Topical Manuka Honey
• Medical-grade Manuka (UMF 10+ or higher) boasts natural hydrogen peroxide activity.
• Apply a thin layer, cover with non-stick gauze.
Studies show Manuka can inhibit S. aureus and speed epithelial repair.
6.3 Tea-Tree Oil Dilution
• Combine 1–2 drops tea-tree oil with 1 Tbsp carrier oil (jojoba or olive).
• Dab on intact skin around the lesion (never straight into an abscess).
Tea-tree carries broad-spectrum antimicrobial properties.
6.4 Immune-Friendly Nutrition
• Load up on omega-3s (salmon, chia) and polyphenols (berries, green tea).
• Cut back on refined sugar, which fuels systemic inflammation
Join our Inflammation Nation Community.
6.5 Stress-Down, Sleep-Up
Cortisol spikes impair wound healing; 7–9 hours of sleep supports immune surveillance. Meditation, gentle yoga, or even a TikTok dance break lowers cortisol. Check out Healing Space sponsored by UCB, to find your zen.
Remember: “natural” doesn’t always mean “harmless.” Patch-test new topicals and inform your physician. See community-recommended products here.
7. Everyday Wound Care to Block Incoming Infections
- Cleanse Gently. Use a pH-balanced, fragrance-free cleanser once or twice a day.
- Skip the Germ-Nukes. Over-using antibacterial soap wipes out good skin flora.
- Pat Dry—Don’t Rub. Friction can rupture fragile tissue.
- Non-Stick Dressings. Silicone mesh or hydrocolloid pads trap moisture just enough to aid healing.
- Switch Dressings Daily or after each drainage event.
- Laundry Hygiene. Wash towels and clothing in hot water; add white vinegar for extra germ kill.
8. Medical Therapies When Infection Is Confirmed
• Oral Antibiotics.
• Topicals.
• Pain Management.
Read more on Medication Treatments for Hidradenitis Suppurativa.
9. Living with HS: Tips for Lowering Overall Infection Risk
• Invest in Breathable Fabrics. Cotton, bamboo, or moisture-wicking athletic gear
• Regular Dermatology Check-Ins. Early intervention = fewer complications. Find a derm with HS experience on our derm finder.
10. Bottom Line: Precision Prevents Problems
Calling every HS flare a skin infection is like calling every square a rectangle—technically possible, practically confusing. Understanding the difference between inflammation-driven HS abscesses and actual bacterial skin infections lets you:
- Seek the right treatment faster (antibiotics for infection, anti-inflammatories for HS).
- Avoid antibiotic overuse and the gnarly resistance that follows.
- Advocate for yourself with healthcare providers who may still equate pus with infection 100% of the time.
So the next time someone points at your HS lesion and whispers “That looks infected,” you can smile, drop some science, and get back to living your life—armed with a clear plan for both prevention and care.
Need More Support?
• Dive into our comprehensive HS Wound-Care Guide.
• Join the HS Connect Community Forum for real-time tips and solidarity.
• Follow @HSConnectorg on your favorite social media platform
Medical Disclaimer
The information provided by HS Connect (“we,” “us,” or “our”) on this website HSConnect.org] (the “Website”) is for general informational purposes only. All content, including text, graphics, images, and information, is presented as an educational resource and is not intended as a substitute for professional medical advice, diagnosis, or treatment.
Please consult with a qualified healthcare provider before making any decisions or taking any action based on the information you find on this Website. Do not disregard, avoid, or delay obtaining medical or health-related advice from your healthcare provider because of something you have read on this Website.
This Website does not recommend or endorse any specific tests, physicians, products, procedures, opinions, or other information that may be mentioned on this website. Reliance on any information provided on the Website, its content creators, or others appearing on the website is solely at your own risk.
If you think you may have a medical emergency, call your doctor, go to the nearest emergency department, or call emergency services immediately. We are not responsible for any adverse effects resulting from your use of or reliance on any information or content on this Website.
By using this Website, you acknowledge and agree to this disclaimer in full.
References
- Jemec, G. B. E. (2012). Clinical practice. Hidradenitis suppurativa. New England Journal of Medicine, 366(2), 158–164. https://doi.org/10.1056/NEJMcp1014163
- Alikhan, A., et al. (2019). North American clinical management guidelines for hidradenitis suppurativa. Journal of the American Academy of Dermatology, 81(1), 76–90. https://doi.org/10.1016/j.jaad.2019.02.067
- Kirby, J. S., & Grice, E. A. (2020). The skin microbiome in hidradenitis suppurativa: A review. Dermatologic Clinics, 38(3), 365–377. https://doi.org/10.1016/j.det.2020.03.001
- Kunjadić, N., et al. (2023). Culture versus 16S rRNA sequencing for bacterial identification in HS lesions. Dermatology, 239(5), 742–750. https://doi.org/10.1159/000528264
- Goldburg, S. R., et al. (2020). Current understanding of the inflammatory pathways in hidradenitis suppurativa. Journal of the American Academy of Dermatology, 82(5), 1061–1072. https://doi.org/10.1016/j.jaad.2020.01.002
- Tzellos, T., et al. (2021). European S1 guideline for the treatment of hidradenitis suppurativa—Update 2021. Journal of the European Academy of Dermatology and Venereology, 35(12), 1969–1999. https://doi.org/10.1111/jdv.17509
- Mayo Clinic. (2024). Boils and carbuncles. Retrieved August 15, 2025, from https://www.mayoclinic.org/diseases-conditions/boils-and-carbuncles
- Centers for Disease Control and Prevention. (2024). Methicillin-resistant Staphylococcus aureus (MRSA). https://www.cdc.gov/mrsa
- Somayaji, R., et al. (2021). Incidence and outcomes of cellulitis in chronic inflammatory skin disease. Clinical Infectious Diseases, 73(4), e1036–e1043. https://doi.org/10.1093/cid/ciaa1197
- Carter, D. A., et al. (2016). Therapeutic Manuka honey: Antimicrobial activity against MRSA. AIMS Microbiology, 2(4), 294–312. https://doi.org/10.3934/microbiol.2016.4.294
- Daily, J. W., et al. (2021). Topical curcumin for skin inflammation: A systematic review. Phytotherapy Research, 35(3), 1371–1381. https://doi.org/10.1002/ptr.6907
- Hammer, K. A. (2023). Antimicrobial properties of tea-tree oil: An updated review. Clinical Microbiology Reviews, 36(1), e00232-22. https://doi.org/10.1128/cmr.00232-22
- World Health Organization. (2024). AWaRe classification: Antibiotic stewardship resources. https://www.who.int/teams/integrated-health-services/antimicrobial-resistance/aware
- van der Zee, H. H., et al. (2020). The microbiome of hidradenitis suppurativa: A systematic review. Experimental Dermatology, 29(8), 702–715. https://doi.org/10.1111/exd.14195
- Ring, H. C., et al. (2017). Bacterial biofilms in hidradenitis suppurativa: A case–control study. British Journal of Dermatology, 177(4), 1132–1134. https://doi.org/10.1111/bjd.15462
- Wound, Ostomy and Continence Nurses Society. (2023). Clinical guidelines for wound cleansing and dressing selection. https://www.wocn.org/practice-resources
- FDA. (2023). Guidance on over-the-counter topical antiseptics. https://www.fda.gov
