By: Cristina Curp, HS Patient Advocate, NTP
What Is the Hurley Staging System, and Who was Hurley?
Let’s start at the beginning. The Hurley clinical staging system is a simple, three‑stage classification developed by dermatologist H.J. Hurley in 1989 to help clinicians describe HS severity based on visible lesions; without needing fancy tests or complicated scoring systems.
Hurley introduced this model in a dermatologic surgery text to guide treatment decisions, especially surgical ones, using three distinct levels: mild, moderate, and severe HS. And that’s why, almost 35 years later, we still rely on it; it’s straightforward, reliable, and frequently referenced in studies and clinical guidelines.
There are three stages to assess severity, with possible in-between stages where you may experience more severe symptoms without tunnel formation. Different body areas can also show varying stages (e.g., stages 1 in the armpits, stage 2 in the groin). It is important to note that disease progression is not guaranteed, but it may happen.
Hurley Stage 1 (Mild HS)
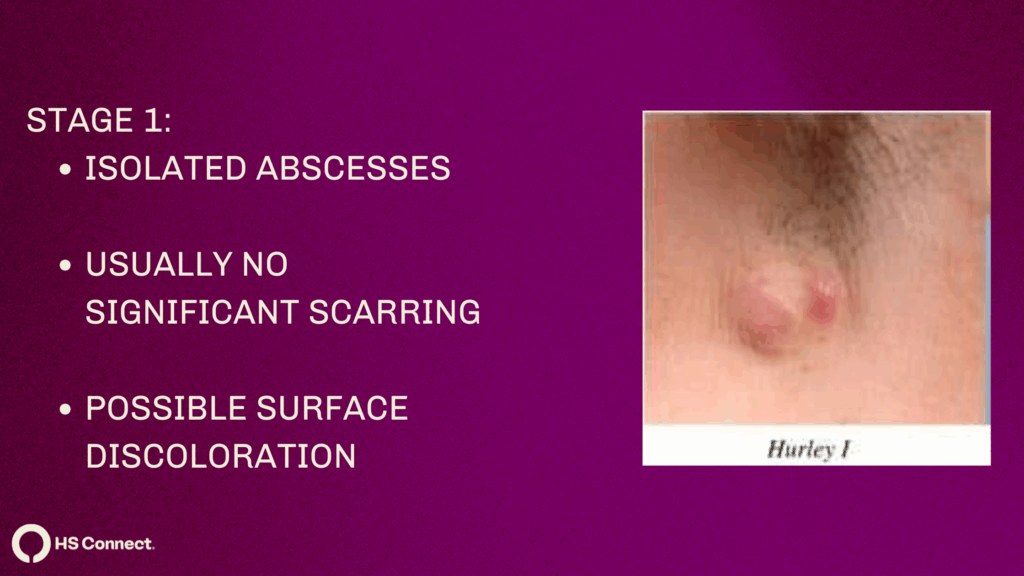
What Does It Look Like?
- You might see one or a few isolated inflamed abscesses (or nodules). Often seen in folds like the armpits, groin, or under the breasts, but may occur anywhere there is a fair follicle
- Importantly: no tunnels (sinus tracts) under the skin, and minimal scarring, possible discoloration after healing.
How Common Is It?
- Many surveys estimate that over two‑thirds of people with HS fall into Stage I.
What Can You Do at Stage 1?
This stage is all about control and prevention:
1. Topical therapies – antibiotics like clindamycin to reduce inflammation.
2. Lifestyle tweaks – wear loose clothes, keep skin cool and dry, avoid friction. Keep a journal to find out your triggers (can be stress, foods, fabrics, soaps, etc).
3. Oral meds – short antibiotic courses (tetracyclines), maybe hormonal treatments if cycles or hormones play a role.
4. Self‑care routines – warm showers, antiseptic washes, gentle skin care. Product Recommendations
5. Laser Hair Removal- Hair follicles are key in HS pathogenesis and all included studies showed a significant improvement in HS disease severity after LHR regardless of the laser device used, likely related to hair follicle unit destruction (source). – Prior Authorization Templates
What to Say to Your Doctor
- “I’ve had a few painful lumps in one area, but they heal without scarring or tunnels.”
- “I want to begin early treatment to avoid more severe stages.”
- Ask: “Could topical treatments or lifestyle changes work for me?”
- “Am I a good candidate for laser hair removal?”
Hurley Stage II (Moderate)
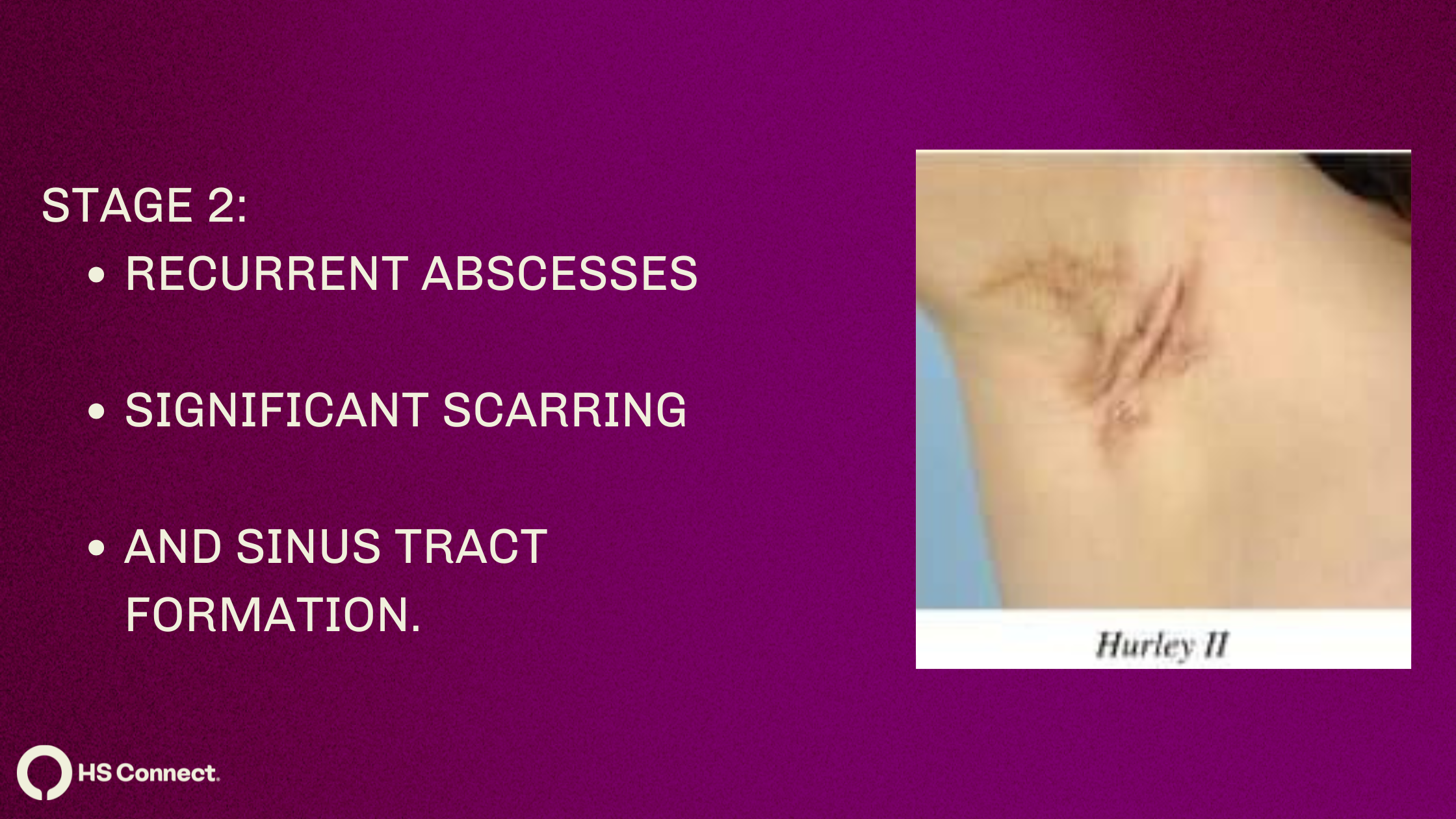
What does it look like?
- Stage II is marked by recurrent abscesses and nodules, often more than one area, now with tunnel forming and early scarring.
- Lesions may be widely separated but leave more obvious tracks and heal with fibrotic marks.
How common?
- Estimates suggest around 28% of HS patients are Stage II.
Why it matters:
- This stage crosses the line from mild to moderate, it signals a more active disease process that won’t just go away on its own.
Treatment strategies:
- Oral antibiotics (like rifampin + clindamycin combos) for longer stretches.
- Hormonal/antiandrogen agents (e.g. spironolactone, finasteride) if hormonal patterns show up.
- Local procedures like:
- Intralesional triamcinolone injections
- Deroofing of painful flares (deroofing videos).
- Biologics: FDA‑approved adalimumab or newer options like secukinumab for more stubborn cases.
What to say to your doctor:
- “There are multiple painful bumps in various areas that recur, and I notice tunnels and scars.”
- Ask: “Should we consider biologics? Would a hormone evaluation help?”
- Ask “What about deroofing the stubborn flares?”
Hurley Stage III (Severe)
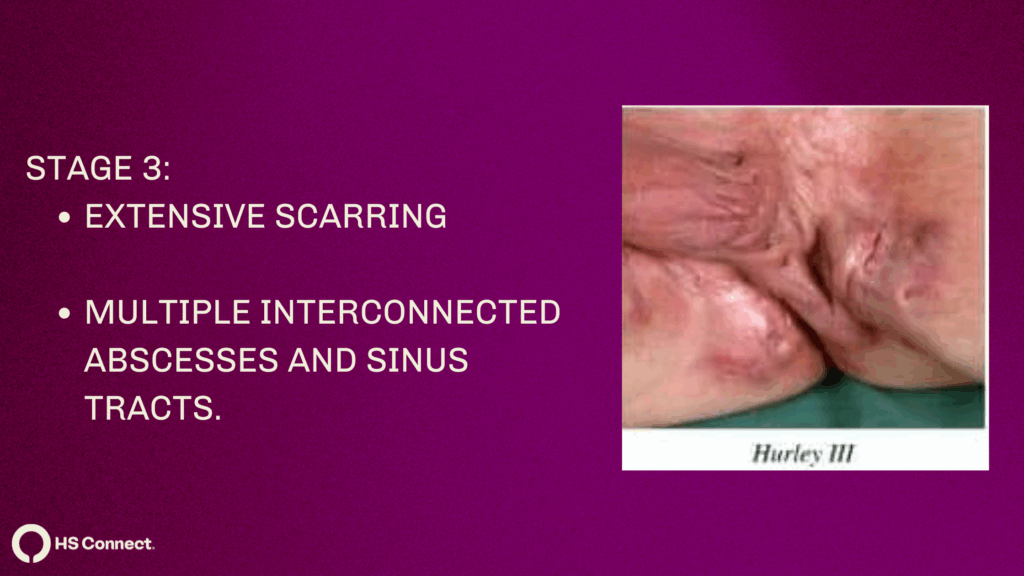
What does it look like?
- In Stage III, HS is diffuse; multiple, interconnected sinus tracts, abscesses, and extensive scarring throughout an entire region.
- The skin can appear like a network of tunnels and scars that can leak drainage, and be very, very painful.
How common?
- Stage III is the least common, affecting roughly 4–29% of people with HS, depending on the clinic.
Why it matters:
- This is the most challenging phase. There’s a real risk of complications: chronic pain, mobility issues, anemia, arthritis, even rare skin cancer. It is very important to seek treatment.
Treatment strategies:
1. Systemic medications – biologics like adalimumab or secukinumab, immunosuppressants
2. Surgical options, tailored to lesion extent:
- Wide excision – removing entire areas of affected skin.
- Deroofing – shaving off tunnel tops.
- Skin grafts or flaps to close defects.
- Laser therapy for hair removal and lesion reduction.
- You can read more on surgical treatments here.
3. Supportive measures – pain management, wound care, psychosocial support.
What to say to your doctor:
- “I have widespread lesions with tunnels and scars across an entire region.”
- Ask: “Is surgery appropriate now? Should I be on biologic or combination therapy? Can we arrange a referral for surgical evaluation?”
Why Hurley Staging Matters
1. It guides treatment
- Dermatologists often start with topicals for Stage I, escalate to antibiotics and biologics for Stage II, and consider surgery or full‑blown systemic therapy for Stage III. However, at HS Connect we have “a why wait?” mindset. We know antibiotics are not effective long term, and starting a biologic can help the disease not progress. Link to treatment options article.
- Deroofing procedures can be done at any stage to resolve a flare. Do not do I&D’s, they have 100% recurrence rate. See our article on that HERE.
2. It helps with communication
- Telling your doctor “I’m at Hurley Stage II” clearly communicates how serious your HS is and what kind of interventions should be discussed.
3. It sets realistic expectations
- Each stage has a known prognosis. Early interventions in Stage I might prevent progression. Stage III often requires combined approaches and longer healing processes.
Talking to Your Doctor—Your HS Game Plan
Use this conversational roadmap during appointments:
1. Describe symptoms clearly
- “I’ve had inflamed lumps that healed without scarring until recently, when I noticed drainage and tunnels.”
2. Ask for staging
- “Can you tell me which Hurley stage I’m in? How does my stage affect treatment choices?”
3. Set goals together
- If Stage I: “I want to prevent progression—what should be my next steps?”
- If Stage II: “Are antibiotics enough, or should we try a biologic?”
- If Stage III: “I’d like your thoughts on surgery—what types and risks are involved?”
4. Discuss lifestyle support
- HS care isn’t just meds and surgery. Talk about:
- Clothing adjustments, diet, friction avoidance
- Specialty underwear, antiseptic washes
- Mental health: HS Connect peer groups, counseling, body image support – Healing Space
Beyond Hurley: A Smarter Approach
While the Hurley system remains widely used, it’s not perfect. It doesn’t capture flare frequency, pain levels, or how HS impacts daily life.
In research settings, tools like:
- Sartorius Score – detailed count of regions, lesions, and scar/tunnel distances.
- HS‑PGA or HiSCR – evaluate global disease improvement, particularly in trials.
- DLQI – gauges quality of life impact, especially for emotional and social aspects.
But in most clinic appointments, Hurley is fast, familiar, and effective, so it remains a top choice for staging and planning.
To Sum It Up
The Hurley staging system is a cornerstone for classifying HS severity, guiding treatments from Stage I through III.
- Understanding what your stage means, lesion types, tunnel formation, scarring, helps you take informed steps with your healthcare team.
- Use clear, stage-based language with your doctor. Ask about specific treatment options, from topicals and lifestyle tweaks to antibiotics, biologics, or surgery.
- Don’t underestimate the emotional and social impact of HS. Tools like HS Connect, peer support, and mental health conversations matter, too.
By getting familiar with the Hurley stages, you can work with your dermatologist or HS specialist to create a personalized, proactive treatment plan—one that focuses on both symptom control and quality of life.
Medical Disclaimer
The information provided by HS Connect (“we,” “us,” or “our”) on this website HSConnect.org] (the “Website”) is for general informational purposes only. All content, including text, graphics, images, and information, is presented as an educational resource and is not intended as a substitute for professional medical advice, diagnosis, or treatment.
Please consult with a qualified healthcare provider before making any decisions or taking any action based on the information you find on this Website. Do not disregard, avoid, or delay obtaining medical or health-related advice from your healthcare provider because of something you have read on this Website.
This Website does not recommend or endorse any specific tests, physicians, products, procedures, opinions, or other information that may be mentioned on this website. Reliance on any information provided on the Website, its content creators, or others appearing on the website is solely at your own risk.
If you think you may have a medical emergency, call your doctor, go to the nearest emergency department, or call emergency services immediately. We are not responsible for any adverse effects resulting from your use of or reliance on any information or content on this Website.
By using this Website, you acknowledge and agree to this disclaimer in full.
