By: Cristina Curp, HS Patient Advocate, NTP
If you’ve got hidradenitis suppurativa (HS), you’ve probably heard this one before: “Have you tried antibiotics? What about Humira? Maybe birth control?” It can feel like the wild west of treatments out there, with everyone throwing something different at you. HS is tricky. It’s not like a regular skin condition where one cream magically fixes it all. It’s a full-body, inflammatory condition that needs a plan, and for many of us, that plan includes medication.
The good news is there are more options now than ever before. It’s not perfect, and we’re still waiting for that “one size fits all” miracle cure, but understanding the tools we do have makes a huge difference. Let’s walk through some of the main medications doctors use for HS so you can have a better idea of what might be right for you

Topical Treatments
If you’re early in your HS journey or have mild flares, your doctor might start you with something topical, meaning it goes on your skin.
Clindamycin is the most common. It’s an antibiotic gel or lotion that helps calm down inflammation and kill off bacteria. Then there’s resorcinol cream, which is a bit of an unsung hero. It’s technically used “off-label,” but it’s great for unclogging pores and reducing painful swelling. Think of it like giving your angry skin a little spa treatment (minus the cucumber water).
Topicals can help, but they’re often not strong enough for moderate or severe HS on their own. They’re usually the opening act, not the headliner.
Oral Antibiotics
When things get more intense, doctors may bring in antibiotics you take by mouth. These aren’t just about killing bacteria. Many of these medications, like doxycycline or minocycline, also reduce inflammation, which is a big deal for HS.
Sometimes you’ll hear about the clindamycin and rifampin combo. It’s a power duo for moderate HS and can be really effective. There are also other antibiotics your doctor might choose based on what bacteria is hanging around.
Are antibiotics a forever thing? Usually not. They’re more like “break glass in case of flare” treatments, or they’re used alongside other medications.
Hormonal Treatments
For many women with HS, hormones are like that frenemy who always shows up uninvited. If your flares seem to follow your cycle, hormone-based treatments can be game-changers.
Spironolactone is an anti-androgen medication that helps calm down hormonal triggers. And certain birth control pills can help even things out. It’s not magic, but for some people, this is the key to fewer and less painful breakouts.
Biologics
Welcome to the big leagues. Biologics are the heavy hitters used for moderate to severe HS. These are injections that target the overactive immune response causing all the drama in your skin.
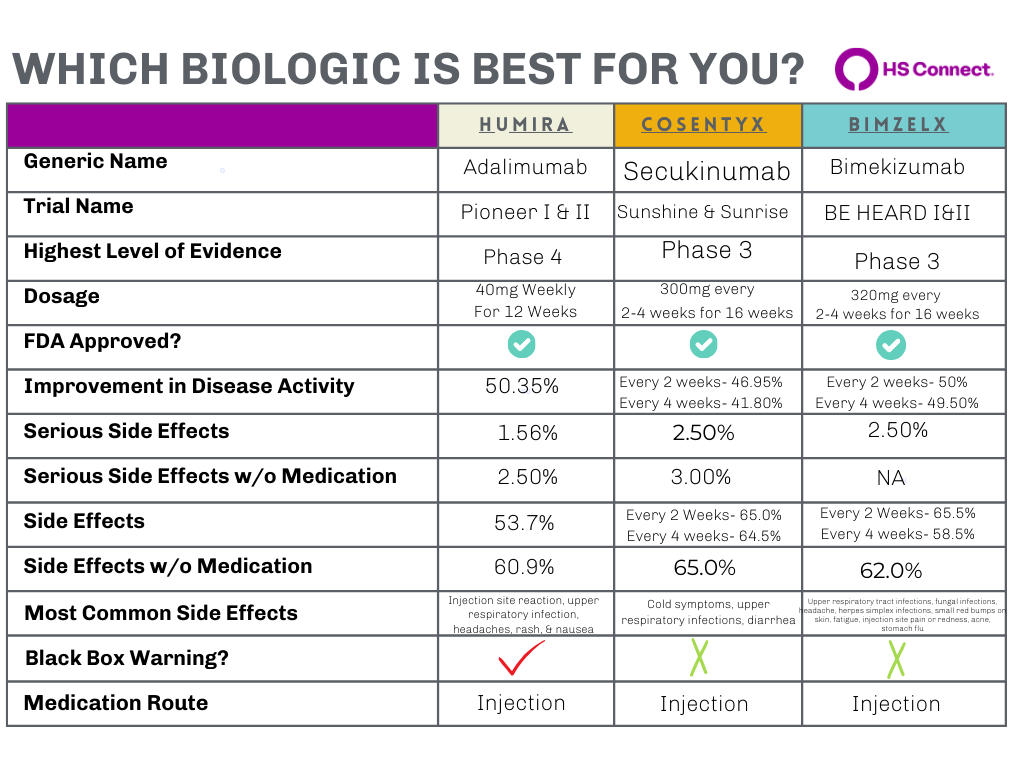
You’ve probably heard of Humira (adalimumab). It was the first FDA-approved biologic for HS and is still the most widely used. Cosentyx (secukinumab was approved by the FDA for the treatment of moderate to severe hidradenitis suppurativa (HS) in adults, this approval was granted in October 2023. But now there’s a newer player: Bimzelx (bimekizumab), which got FDA approval in November 2024, for treatment of adults with moderate to severe hidradenitis suppurativa (HS). This approval marks Bimzelx as the first and only approved medication that specifically targets and inhibits both interleukin (IL)-17A and IL-17F cytokines, which are believed to play a role in the inflammation associated with HS. There’s also Remicade (infliximab), which isn’t officially approved for HS but is sometimes prescribed when other treatments fail. (1, 2)
Biologics can be life-changing for some people, but they’re not a quick fix. They take time, and they require regular injections and bloodwork. And let’s be real, they can be expensive. Thankfully, there are assistance programs to help with cost, which is something HS Connect can help you navigate (coming soon!).
Other Medications
Sometimes doctors will reach for corticosteroids (like prednisone) during really bad flares. These can calm inflammation fast, but they’re not meant for long-term use because the side effects can be intense. Think of steroids as the fire extinguisher, helpful in emergencies, but you don’t want to use them every day.
Pain Management
If you know HS, you know pain. Managing it is just as important as treating the disease itself.
NSAIDs like ibuprofen or naproxen can take the edge off both pain and swelling. Beyond that, some people find relief with nerve pain medications, physical therapy, or even just simple things like heat packs, ice packs or Epsom salt baths. Pain management is personal and often takes a little experimenting to find what works for you.
GLP-1 Medications
This is a newer topic in the HS world. GLP-1 medications (like semaglutide) are mostly used for diabetes and weight management, but some people with HS have noticed improvements while taking them. The research isn’t there yet, but early signs are interesting, read more here. Basically, it’s something worth keeping an eye on.
Talking to Your Doctor
Here’s the part that can feel intimidating, asking your doctor about these options. But remember, you’re the expert on your own body.
Bring notes about your flares, pain levels, and what you’ve tried so far. Ask about combination treatments, because for many of us, it takes more than one medication to get things under control. And if your doctor doesn’t seem up to speed on HS, it’s okay to get a second opinion or find a specialist. HS Connect has a list of resources to help with that too. Check out our Derm Finder here.
Medical Disclaimer
The information provided by HS Connect (“we,” “us,” or “our”) on this website HSConnect.org] (the “Website”) is for general informational purposes only. All content, including text, graphics, images, and information, is presented as an educational resource and is not intended as a substitute for professional medical advice, diagnosis, or treatment.
Please consult with a qualified healthcare provider before making any decisions or taking any action based on the information you find on this Website. Do not disregard, avoid, or delay obtaining medical or health-related advice from your healthcare provider because of something you have read on this Website.
This Website does not recommend or endorse any specific tests, physicians, products, procedures, opinions, or other information that may be mentioned on this website. Reliance on any information provided on the Website, its content creators, or others appearing on the website is solely at your own risk.
If you think you may have a medical emergency, call your doctor, go to the nearest emergency department, or call emergency services immediately. We are not responsible for any adverse effects resulting from your use of or reliance on any information or content on this Website.
By using this Website, you acknowledge and agree to this disclaimer in full.
