If you’re living with polycystic ovary syndrome (PCOS) and your skin seems to have a mind of its own, you’re not imagining things. Breakouts, bumps, scars, and flare-ups can all be part of the PCOS package, but here’s the thing: not all skin changes are “just hormonal acne.”
Some skin symptoms in PCOS signal something deeper, like hidradenitis suppurativa (HS) or other inflammatory conditions. Understanding what’s normal—and what needs a closer look—can help you manage symptoms and get the right care.
At HS Connect, we live at the intersection of hormones, inflammation, and skin health. Let’s break down what’s happening beneath the surface.
What “PCOS Skin” Really Means
PCOS affects up to 10% of women of reproductive age and is caused by hormonal imbalances—most notably, higher-than-normal levels of androgens (sometimes called “male hormones,” though everyone produces them) ¹. These elevated hormones can make your skin oilier, clog pores more easily, and drive inflammation.
Common PCOS Skin Symptoms
- Cystic acne – deep, painful breakouts, usually on the jawline, chin, and neck
- Excess oil production – even after multiple cleansers and blotting sheets
- Hirsutism – coarse, dark hair growth on the chin, upper lip, chest, or stomach
- Thinning hair or androgenic alopecia – scalp shedding or widening parts
- Acanthosis nigricans – dark, velvety skin patches, often under the arms or around the neck
- Seborrhea – oily, flaky skin on the scalp, eyebrows, and sides of the nose
These symptoms are classic signs of hormonal imbalance, but if you’re also noticing recurring nodules, painful abscesses, or scarring in areas like the armpits or groin, it could be more than PCOS acne.
When It’s More Than “Hormonal Acne”
Hormonal acne is a hallmark of PCOS, but other inflammatory skin conditions—especially hidradenitis suppurativa (HS); can appear alongside it. Knowing the difference matters because treatments for acne and HS are not the same.
1. Hormonal Acne: The Usual Suspect
Hormonal acne tends to:
- Show up around the jawline, chin, neck, and sometimes upper back
- Worsen right before your period
- Respond (at least somewhat) to traditional acne treatments, though flare-ups may persist
Research shows that elevated androgens drive excess oil production and clogged pores, which leads to these deeper, cystic breakouts ².
2. Hidradenitis Suppurativa (HS): The Overlooked Connection
While HS isn’t caused by PCOS, studies have found that women with PCOS are significantly more likely to develop HS ³. Both conditions involve hormonal, metabolic, and inflammatory pathways, which explains the overlap.
Signs your “acne” might actually be HS:
- Painful, inflamed nodules in the armpits, groin, under breasts, or buttocks
- Recurring abscesses that don’t heal well
- Scarring and tunnels (sinus tracts) under the skin
- Flares that don’t respond to acne treatments
If this sounds familiar, it’s worth bringing up HS with your dermatologist or gynecologist.
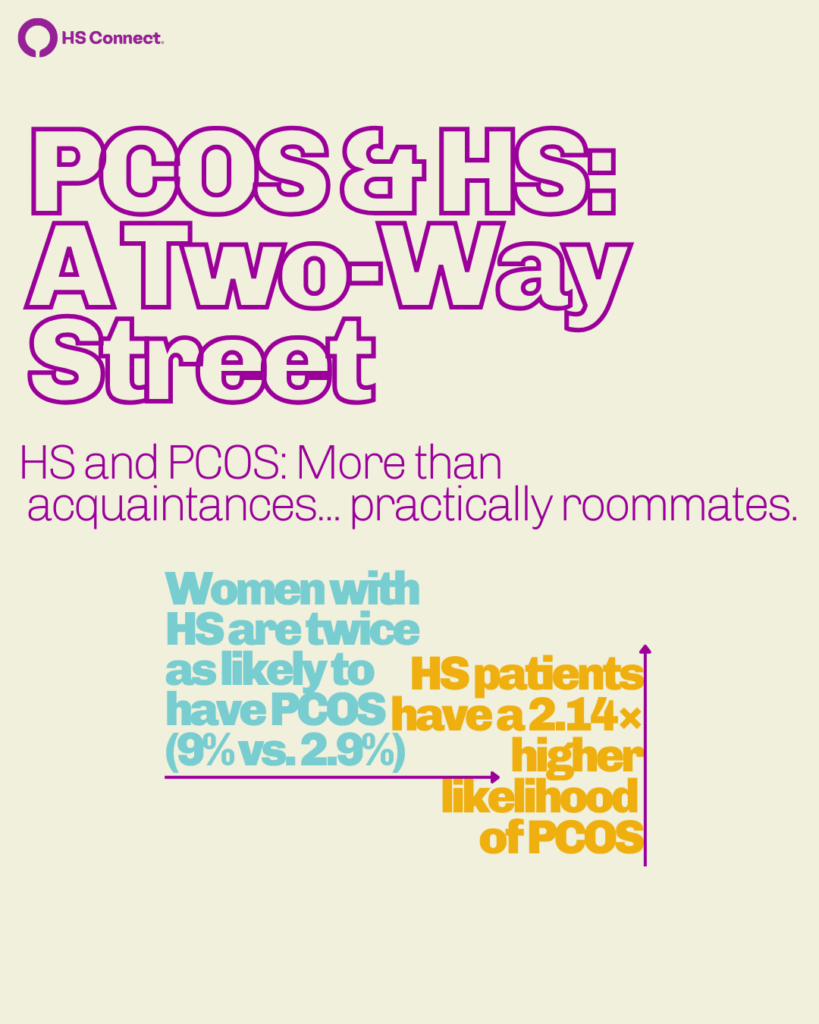
The Science Behind the PCOS-HS Link
Several studies have highlighted the connection between PCOS and HS:
- A 2021 population-based analysis found that women with HS were nearly twice as likely to have PCOS compared to those without HS ².
- A 2023 review noted that shared pathways—like insulin resistance, obesity, and chronic inflammation—may explain why the two conditions often coexist ³.
- Emerging research also suggests that anti-androgen therapies (like spironolactone) may improve both acne and HS symptoms in some PCOS patients ⁴.
The takeaway? If you have PCOS and HS-like skin symptoms, they may share the same hormonal drivers, but require different treatment strategies.
Treatment Options for PCOS Skin (and When HS Changes the Plan)
The right treatment depends on whether you’re dealing with hormonal acne, HS, or both. Here’s an overview of options to discuss with your provider:
For Hormonal Acne and Hirsutism
- Topical treatments – benzoyl peroxide, retinoids, and azelaic acid
- Oral contraceptives – regulate cycles and lower androgen levels
- Spironolactone – an anti-androgen that can improve acne and hair growth ⁴
- Laser hair removal or electrolysis – especially effective for PCOS-related hirsutism
For Hidradenitis Suppurativa
- Topical antiseptics or antibiotics – for mild HS
- Oral medications – including antibiotics, hormonal therapy, and sometimes metformin
- Biologics – like adalimumab, for moderate-to-severe HS
- Lifestyle approaches – weight management, anti-inflammatory diets, and smoking cessation can all improve outcomes ³
Because PCOS and HS often share underlying hormonal and metabolic roots, a combined approach—addressing inflammation, insulin resistance, and androgens—tends to work best.
HS Symptoms to Watch for if You Have PCOS
If you have PCOS and experience any of the following, it’s worth asking your provider about HS:
- Tender, swollen nodules in skin folds
- Painful abscesses that drain or recur
- Scarring or “tunnels” under the skin
- Flare-ups that don’t improve with standard acne treatments
Early diagnosis and treatment can make a huge difference in preventing long-term scarring and improving quality of life.
FAQs About PCOS Skin
Q: How do I know if my acne is from PCOS or something else?
If your breakouts are deep, cyclical, and focused on the jawline, PCOS may be the cause. Lab testing can confirm if high androgens are driving your symptoms.
Q: What’s the connection between PCOS and HS?
Studies show women with HS are significantly more likely to have PCOS. Both involve hormonal imbalances, inflammation, and insulin resistance, but HS requires its own treatment strategy.
Q: Can PCOS skin problems improve?
Yes—with the right approach. Managing hormones, reducing inflammation, and addressing insulin resistance can all improve acne, HS flares, and related symptoms over time.
Q: Will supplements help with PCOS skin?
Emerging research suggests that compounds like N-acetylcysteine (NAC), selenium, and alpha-lipoic acid (ALA) may improve acne in PCOS ⁵, but more studies are needed. Always check with your provider before starting supplements.
The Bottom Line
Not every PCOS skin symptom is “just hormonal acne.” If you’re also dealing with painful nodules, abscesses, or scarring, it could be hidradenitis suppurativa—and that changes the game.
Understanding the difference means better treatment, less frustration, and improved long-term outcomes. At HS Connect, we believe knowledge is power, and you deserve answers (and relief).
Sources:
[1] https://pubmed.ncbi.nlm.nih.gov/40386061/
[2] https://pubmed.ncbi.nlm.nih.gov/33493574/
[3] https://pubmed.ncbi.nlm.nih.gov/37982912/
[4] https://pubmed.ncbi.nlm.nih.gov/37121475/
[5] https://pubmed.ncbi.nlm.nih.gov/40386061/
Medical Disclamer
This content is for educational and informational purposes only. It is not intended to provide medical advice, diagnosis, or treatment. Always consult with a qualified healthcare provider about any questions or concerns you may have regarding a medical condition, including PCOS, hidradenitis suppurativa, or other skin and hormonal health issues.
